News
Cancer cell ‘decathlon’ to help predict tumour aggressiveness and metastasis
We celebrate the one-year anniversary of an ongoing research project funded by the European Innovation Council which aims to quantify a cancer cell’s ability to respond to environmental stress that threatens its survival, a key indicator of tumour progression and aggressiveness.
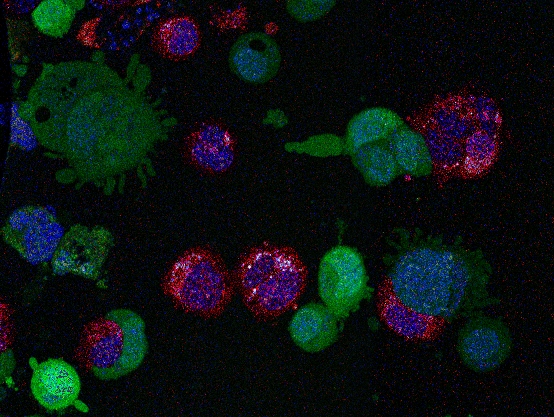
Credit: Chiara Cannatá, IMIM & Fabio Pezzano, CRG
In response to changing environments that threaten their survival, cancer cells have an extraordinary ability to change their behaviour, shape and function. This trait, a key indicator of tumour progression and aggressiveness also known as cell plasticity, allows cancer cells to adapt to stress and keep growing.
Cell plasticity is fundamental for cancer’s ability to cheat death. For example, cells can switch to using old and damaged parts to keep functioning or activate cellular programs that freeze them in a state of senescence. Cells can also detach from a primary tumour and invade other tissues, contributing to metastasis, even with the body normally inducing cells to self-destruct in the absence of proper cell-to-cell interactions.
Despite playing a central role in cancer progression, there is no universal consensus on the definition of cell plasticity. Being able to quantify the impact of these mechanisms would be a huge boon for cancer research and treatment, paving the way for new tools that predict how aggressive a tumour is and at the same time, boost the development of more effective and personalized cancer therapies.
“When cancer cells attempt to relocate to a new part of the body to metastasise, they have to overcome a series of challenges. It’s like a decathlon at cellular scale, but instead of swimming, running or jumping, cancer cells have to physically squeeze through spaces, adapt to different chemical and physical environments or interact with new types of cells when changing locations in the body. If we could quantify the cellular ‘fitness’ in these events like in a scoring system used in sports, we could predict tumour aggressiveness and metastatic potential” says ICREA Research Professor Verena Ruprecht, researcher at the Centre for Genomic Regulation (CRG) in Barcelona.
An international consortium led by Dr. Ruprecht aims to tackle this longstanding challenge by developing a new technology platform which can quantitatively assess tumour plasticity at the single cell level. Dubbed PLAST_CELL, the technology will mimic the physiological stresses that naturally occur in the human body and provide quantitative readouts on a cell’s shape, proliferation and survival and molecular features associated to its capacity to adapt to different environments.
“We will create a high-resolution live-imaging microscope which will be connected to a device that can mimic the stress that cancer cells face when proliferating and colonizing different organs, including the mechanical ‘squeezing’ of cells in dense tissues or during migration” explains Dr. Ruprecht. “With this information, we can study cancer cells with known low or high metastatic potential. The images result in the creation of datasets that will feed AI tools and ultimately help predict the metastatic potential of cancer samples from patients.”
The live-imaging microscope will be used to set quantitative standards to identify genetic, molecular, and biophysical mechanisms underlying cancer cell plasticity and tumour aggressiveness. The consortium believes the platform will give rise to ‘Plastomics’, an entirely new field in biology which can provide a new perspective in cancer analysis, diagnosis and – in the future – treatments. The researchers anticipate that pharmaceutical drug discoveries targeting metastatic potential and resistances will emerge based on PLAST_CELL within a ten-year period. The platform also aims to be adopted in the clinic as a new and powerful diagnostic tool to assess tumour aggressiveness.
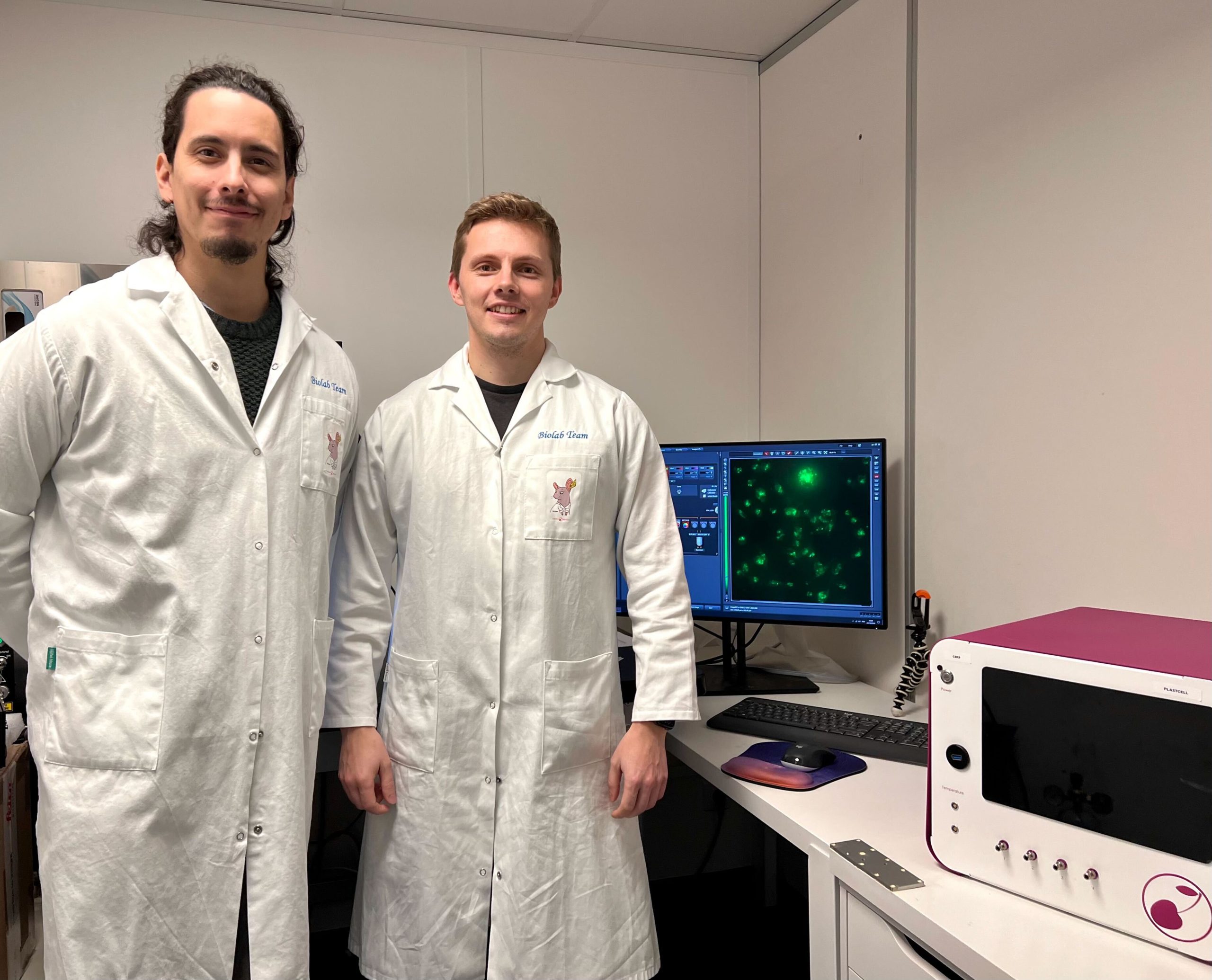
The PLAST_CELL team
The project is coordinated by ICREA Research Professor Verena Ruprecht, Group Leader at the Centre for Genomic Regulation, and funded with 3 million euros from the European Innovation Council, a new body introduced by the European Commission to support the commercialization of high-risk, high-impact technologies in the European Union.
Dr. Ruprecht’s team’s expertise is in cell and tissue dynamics and the interrelation between micro-environmental factors and cell function. Her lab combines the study of cellular morphodynamics in the live embryo with biomimetic in vitro assays to identify control mechanisms of single and collective cellular behaviour, essential for the development of the platform for the assessment of cell plasticity.
Dr. Antoni Celià-Terrassa (IMIM) is an expert in cancer metastasis, cancer stem cells and tumour immunology. He pioneered studies on cellular plasticity during metastasis, bridging basic and translational research with innovation towards the clinic in collaboration with industry. He will work with a multidisciplinary team of biologists, oncologists and pathologists at Hospital del Mar, and critically contribute to the characterization of metastatic cells and tumour aggressiveness.
Dr. Pablo Loza Alvarez and Dr. Jordi Andilla (ICFO) are experts in advanced bioimaging using Super Resolution microscopy, structured illumination microscopy (SIM) and single molecule localization microscopy (SMLM) to understand molecular mechanisms of cell migration and polarization. Their lab develops sophisticated data analysis tools and will be responsible for the quantitative live cell imaging and super-resolution microscopy.
Dr. Virginie Uhlmann (EMBL-EBI) has interdisciplinary expertise in applied mathematics, image processing, and computer science. She develops automated microscopy image quantification algorithms blending mathematical models and machine learning, with a focus on computational morphometry, an essential expertise for the development of a predictive model of tumour aggressiveness based on cell plasticity.
The consortium is complemented by Dr. Jeremy Cramer and Dr. Antoni Homs-Corbera at the French SME Cherry Biotech (CHB), leading a team of engineers, physicists and biologists, with a strong R&D background, focusing on developing a biomedical technology (Organ on Chip) for drug discovery and precision medicine. Its mission is to replace animal testing by reconstructing human tissue (Organoids) in vitro for drug testing. Cherry Biotech’s platforms enable pharmaceutical, biotech companies and healthcare providers to recreate immunocompetent human vascularized organ models and tumor microenvironments for better evaluation of their drug candidates inside a standard multiwell plate (Organ on Well).
This project has received funding from the European Union’s HORIZON-EIC-2021-PATHFINDEROPEN programme under grant agreement No 101046620.